Metatarsal Stress Fractures – words by Gold Coast Foot Centres Podiatrist Nelson Pollard
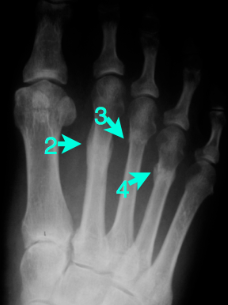
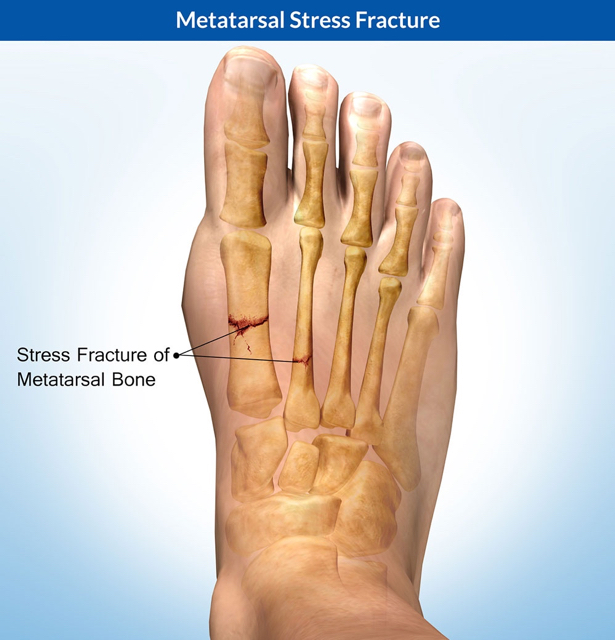 Metatarsal stress fractures are said to be the second most common fracture site, behind the tibia, in the athletic population. Stress fractures of the 2nd, 3rd and 4th metatarsals make up around 90% of metatarsal stress fractures, with fractures of the 2nd being by far the most common. This is thought to be for several reasons such as:
Metatarsal stress fractures are said to be the second most common fracture site, behind the tibia, in the athletic population. Stress fractures of the 2nd, 3rd and 4th metatarsals make up around 90% of metatarsal stress fractures, with fractures of the 2nd being by far the most common. This is thought to be for several reasons such as:
– The 2nd metatarsal is generally longer than the other metatarsals and sits higher on the forefoot parabola, therefore does not share a common axis with any of the other metatarsal heads
– A pronated foot type is thought to be associated. As the foot pronates the 1st MTPJ is dorsiflexed, leaving the 2nd metatarsal head to be the predominant weight bearing structure
– The 2nd metatarsal is also firmly anchored at its base. It is wedged between the medial and lateral cuneiforms, as well as being anchored down by the tarsometatarsal ligaments (short and long plantar ligaments and continuation of the tibialis posterior tendon). This is all said to lead to increased bending forces during activity.
Minimalist shoes and shoes with a lower heel height differential have also shown to increase loading in the plantar forefoot. Although not confirmed, this increase in load through the forefoot may lead to increase incidence of metatarsal stress fractures.
Symptoms and Imaging
Stress fractures are a result of a cumulative load in the tissue which the tissue cannot tolerate and evolve in the following pathway:
– Bone strain: this a dynamic response to stress in the bone. At this stage, there are generally minimal symptoms and changes are only visible on bone scan imaging
– Stress reaction: There is local pain and tenderness. A stress reaction is not visible on plain x-rays
– Stress fracture. There local pain and tenderness with diffuse oedema. A stress fracture can usually be seen on an x-ray 2-3 weeks after the incidence.
As a stress fracture is a result of a cumulative load, rather than an acute occurrence, the onset of pain is gradual, made worse with activity and generally follows a period of increased activity or training intensity. Bone scans can be used as an aid in diagnosing metatarsal stress fractures due to their excellent sensitivity and specificity, although MRI is becoming more advocated due to its fantastic anatomical resolution
Treatment options
Treatment revolves around rest to allow the injured structure to heal. The use of a weight bearing CAM walker, or carbon splint to reduced metatarsal bending is sometimes used. Non-weight bearing x-training is encouraged. Usual training can be recommenced once the fracture site is pain free upon palpation. A monitored and graduated return to sport is required.
Our Physio team will help you – bookings are essential phone 07 5500 6470 or book online