Hip Pain is NOT just Bursitis
Written by GCPSH APA Titled Sports & Exercise Physio, Myles Burfield
 One of the most commonly diagnosed hip injuries is greater trochanteric bursitis, aka ‘The pain in the butt that’s not quite in the butt.’ But has the diagnosis in medical terminology been wrong all this time? Quite possibly!
One of the most commonly diagnosed hip injuries is greater trochanteric bursitis, aka ‘The pain in the butt that’s not quite in the butt.’ But has the diagnosis in medical terminology been wrong all this time? Quite possibly!
How it presents
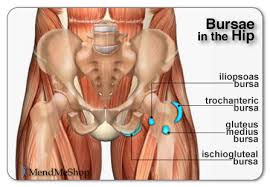
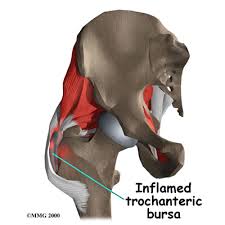
Greater Trochanteric Bursitis, or Greater Trochanteric Pain Syndrome (GTPS) as it’s now more accurately called, is pain that is on the outside of your hip, around your hip bone (see diagram). Pain is local over the site of the bursa, in isolation does not refer down the leg, and is mostly an aching sensation.
How common is it?
It can present in men and women, although due to anatomical variations between sexes it is more prevalent in women. The stats are quite astounding with 1 in 4 women over the age of 50 suffering GTPS, so that’s a 25% chance you’ll get it (sorry ladies). From a physiotherapist perspective, this is especially astounding because it is a condition that is often successfully treated with the correct management. One of the reasons it is so common, and ongoing, is because it is still being diagnosed as ‘bursitis’ when there is another underlying issue causing the bursa to appear inflamed. If treatment is only directed at the bursa, long term resolution of symptoms may not result.
 What does the research say may be the associated underlying issue?
What does the research say may be the associated underlying issue?
As our understanding of tendons and tendinopathy (pathology or an abnormality of the tendon) continues to improve, the medical world has started to evolve the management of conditions that relate to structures that lie close to tendons. Bursa’s are usually located directly beneath tendons and so have inter-linked tissues.
Research is now suggesting most outside hip pain is not primarily due to bursitis, but due to gluteus minimum or gluteus medius mucle tendinopathy PLUS the bursa. Therefore, treatment needs to consist of a thorough examination to check for other factors contributing to your pain, and most likely needs to include treatment of the tendonopathy. Our Physio’s use a tendinopathy model approach for this management.
What is a tendinopathy model approach?
Step 1: Address factors that may be causing additional tension or compression on the tendon.
These could include:
– Tight muscles: Gluteals, ITB, Tensor Fascia Late etc
– Biomechanical factors: Pronating feet, or excessive pelvic sway when walking
– Postural factors: Compression of the tendons (lying on affected side), standing with hips to one side (carrying child)
Step 2: Helping the tendon remodel: This includes a few exercises that encourage the tendon to remodel as a stronger, more resilient tendon. These exercises will start off very basic and then be advanced depending on your physical demands, usually over a number of months.
The bottom line
If you have pain on the side of your hip, it’s probably not just bursitis and it’s worthwhile getting it checked out by your experienced GCPSH physio